I worried about postpartum sex while I was pregnant. Like, when will there be time for sex? or, will my partner think I am me sexy? As soon as I popped this kid out, it became clear that my body and my relationship to my body and my sexuality–to the very wonderful deliciousness that created this child in the first place–had dramatically changed.
I worried about postpartum sex while I was pregnant. Like, when will there be time for sex? or, will my partner think I am me sexy? As soon as I popped this kid out, it became clear that my body and my relationship to my body and my sexuality–to the very wonderful deliciousness that created this child in the first place–had dramatically changed.
There are many better written accounts about the physical trauma of birthing (Chrissy Tiegen or the Body Full of Stars book). What most of them have in common is the shock, the, “Why didn’t anybody tell me about this!?” No sane person would (should?) share with a pregnant woman anything bad that happened to them. And no sane pregnant woman would want to hear about them either. There’s also shame, stigma, and the solitude of going through something hard when it seems everyone else has it easy (which, really, we should know by now is never the case).
I am still not sure what exactly–what information, what mentoring–would have helped me prepare for the bleeding that continues for weeks (like, where does it come from? and why won’t it stop?); the way your breasts feel when a hungry mouth attaches to them, especially one that has a physical challenge and leaves bleeding, achy nipples, and oh man, that sensation when your milk comes in and suddenly you are carrying two solid, heavy stones on your chest; the medical staff demanding a stool from you when the last thing you want if you gave birth vaginally is to feel ANYTHING coming out that route; the actual ripping of flesh, that can rip in many different ways and in different parts and that needs to be sewn up and might be sewn up wrong; the impossibility of sleeping when tired or eating when hungry; the heart-stopping, all-consuming precipice of postpartum depression.
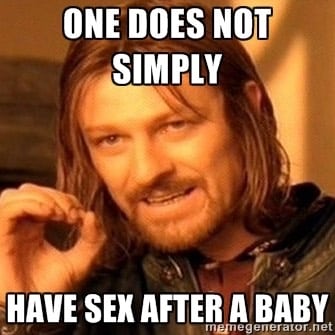
After 6 weeks, when I went to see my OBGYN (because that’s when the medical establishment has decided postpartum “ends”), she said, “all good” and I was super excited for sex– nervous too–and exercise, and to resume tiny bits of pre-baby life.
That night I pounced on my partner as soon as the baby was asleep (for a few hours at least). We fumbled, like newbies, like we’d never had has sex before. But it quickly became clear that something was actually wrong. Not only did it hurt like hell–I sort of expected that–but it just seemed impossible that it would actually go in. As if the space for it had closed. As if there was no hole. We stopped to regroup and figure out if maybe we were doing it wrong. Maybe we forgot how things worked? We tried again. No, for sure for sure, it was physically improbable that anything was going to go in.
Am I the only one who thought that birthing a multiple-pound being would result in stretching rather than tightening?
I asked all the moms I knew: “Did sex hurt?” All but one said, “oh yeah it hurts;” a lot, for a long time, more than a year. For some, the pain didn’t start until later, when they thought they had been spared. Some tried it once and never again. Some just never tried. A dear friend told me to keep trying, through the pain and discomfort. But who on earth enjoys sex when it hurts?!
I wrote to my doctor: “Sex isn’t working.” “Is this normal?” “How do I fix it?” My next appointment revealed that the sutures to close the gash left by my baby’s exit had healed in such a way that they created a barrier of entry. When she showed me in a mirror, it looked like the little bit of tissue that connects the bottom of your tongue to the bottom of your mouth. Like it could be plucked, like a guitar string.

“We can cut it, if you want. Or you can just try stretching by yourself.” Urgh. I was certain I didn’t want another intervention. Also, breastfeeding dries up all the nature moisture from the vagina, so she prescribed an estrogen cream (which I bought but never used because a side effect is cancer).
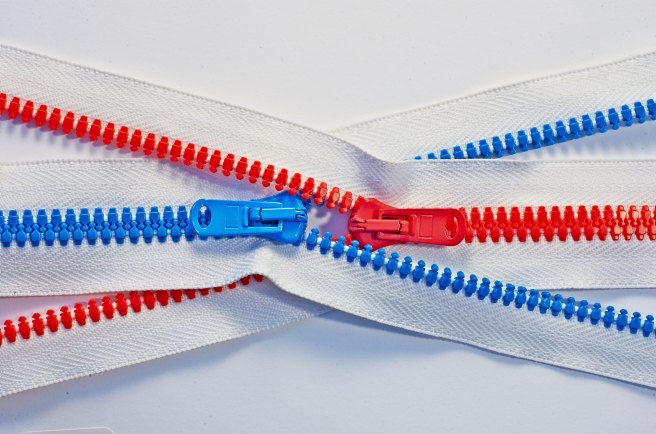
She referred me to a vagina therapist for the internal pain. Ok, that’s not what they are called, but they should be. Pelvic floor therapists focus on the pelvic floor, the muscles, ligaments, and nerves that hold up, like a hammock, your bladder, uterus, vagina, and anus, and help them work well (and like, not fall into one another squishing pee and poop out without your control). In some countries, like France, you get pelvic floor therapy after birth simply because EVERY WOMAN benefits from it (even if there are some sexists reasons why France does it). In the US, though, they make you go through an insane process to “figure out” what is wrong, through loops and loops of paperwork and appointments to find out why sex hurts and why you pee when you sneeze, despite the fact that pelvic floor dysfunction is extremely common, well-studied, and easy to fix through therapy, and incontinence affects 1 in 3 women! They should teach you this when you are a teen, and when you get pregnant, and it should part of postpartum care. WHY IS THIS NOT THE CASE? I read an article from the UK that said that in countries were pelvic floor therapy isn’t common there are tons of products to help women live with incontinence (pads, weird tampon thingies) while little is done to fix this super fixable problem. I wonder why… hmm….someone is making money off women’s suffering.
My vagina therapist said my pelvic floor was just dandy. She said she’d never seen such a productive and strong kegel in a woman who just gave birth (hey, I’ll take a compliment wherever I can get it). The outside tissue had great spring to it, as she depressed it, inch by inch, with a q-tip to test its response. I thought, “Yay!” But a little secret of postpartum (and parenthood in general) is that things might be fine at one point and then not fine at the next. Like, your kid might sleep through the night until 9 months and then something happens and he doesn’t anymore. Your pelvic floor is a living, thriving part of your body and if you are not actively working on it and engaging it, it will slack and make you leak and live in pain. Being fat, having bad posture, my hip and hamstring congenital issues, not working out the muscles that support all of the pelvic area, AND not having rested completely in the first few weeks of postpartum (but really, I want to punch anyone that said that to me, because not everyone has the luxury), all contribute to a further deterioration of the the pelvic floor that results in more pee and more pain. The good news is that, like the rest of our body, it can be improved through exercise and therapy.
The vagina therapist’s assessment of the bad sutures was that I needed to let them heal longer. She said the inside and the outside had healed, but not the middle (she provided no mirror for me to see). She also said that a little stretching would help. “If you bleed, you’ve gone too far.” I really should write to her and ask what she meant by “too far,” like, is it good or is it bad, because that’s what happens every time.
Pain and discomfort make sex undesirable but they aren’t the only challenges to a healthy sex life post-baby. I mean, they are probably the most impactful, given that almost 50% of women with some kind of pelvic floor dysfunction–be it incontinence or pain–avoid intercourse. But besides being so bone-tired that nothing seems sexier than sleep; Besides the soft folds that have taken permanent residence everywhere, and especially my belly, and make me feel unsexy; Besides the mood-killing raspy snores of our baby in the crib at the foot of the bed. Besides all that, sometimes, often, it feels like I just can’t put the right cassette in, or the right CD, or whatever the hell is the millennial equivalent of putting the right tune for the right moment. I just can’t switch in and out of mommahood, and definitely not suddenly. When your boobs are food, it is hard to shift them back to being part of the sexual menu. I can’t be cleaning diapers and praying my child has an easy time going to sleep and then, just like that, become a sexual maven. Quickies, and going from zero to action, are out of the question.
I am struggling to switch the sexy on.
Even masturbation has been a challenge. We live in a tiny studio, so “me time” isn’t a thing in our household. And now, this personal experience feels just a tiny bit icky. How can I muster kinky thoughts and sensations with my child nearby? And asking my husband to take the baby so I can “do” it, just feels wrong. Both my OBGYN and my vagina therapist told me I should be doing lots of self care (and it is among my favorite kinds of sexual expressions), but I just can’t muster the sexual energy. And when I do, it feels almost like cheating to use it up rather than share this energy with my partner. I asked my husband if he could just help me masturbate, that way we could both be together (it counts, right?), but I know that when we make it happen, I will feel so guilty that it will not be fun. Feminist sexual liberation comes to mind–I should focus on my pleasure first and always–but sex is relational to me and it is an important part of our marriage and relationship.

And let’s not forget also about how married sex isn’t the same as fun, single sex. And how sometimes, despite all that he does–and it is a lot–I resent that I bear a bigger burden in child rearing than my husband. And how when we both feel misunderstood and overwhelmed, nobody really wants to have sex. And how birth control can eff your libido up, and even though we use it correctly, I am constantly terrified that I could pregnant. And how we both wish sex could happen without any effort from either one of us.
So what now? Sex impacts our overall quality of life. For me, it is something that has heavily influenced my identity and which made me a mother (I mean, I became a mother by CHOICE because I wanted to and I could, but sex was the vehicle by which that happened).
My plan is first to deal with the physical stuff and then figure out how to deal with the relationship part. Got to strengthen my pelvic floor with squats, clams, hip raises, and yes, kegels. Also, lots of stretching from the video “Down There.” Every day, 3 times a day. I gotta stay focused on exercise, focusing on strength not weight loss because I need my own sexy on. And I gotta get back to acupuncture, massage, and chiropractic work. Perhaps igniting regular, long-standing babysitting relationship would extra helpful now. Therapy might be good, but honestly I don’t have the energy to initiate the process again (go to my OBYGYN, wait 2 months to get an appointment with 1 of 2 therapists in the whole Kaiser SF system dealing with tons of women facing the same issues (again why is this not basic, routine care?), have super long sessions with my child in the room because I wouldn’t have any other way of going). And there’s also some resentment towards a medical system that through it all–pregnancy, birth, and postpartum–has never put my best interest first (and don’t get me started with how badly they were dealing with postpartum depression). I did research pelvic floor reeducation machines, a smaller version of what they use at therapy, and I might get myself one.
The relationship stuff–making the time, channeling the right sexual energy at the right time, waking up the kink–those seem a bit harder to solve, or at least not as well researched and fixable as the physical stuff.
Patience, compassion, honesty, and love will help.
Talking about it feels like a good start.